Hunt Study Shows Thyroid Prevents Heart Attacks by Jeffrey Dach MD
In 1976 Broda Barnes was the first to connect low thyroid function with heart disease in his book
Above Image: Institution of Medicine Under Assault by the Hunt Study which questions their dogma. Courtesy Wikimedia.
How did Broda Barnes discover the connection between low thyroid and heart disease? Barnes took summer vacations in Graz Austria every year to study the autopsy files. Graz had a high prevalence of thyroid disorders, and anyone in Graz who died over the past 100 years required an autopsy to determine cause of death, as mandated by the authorities. This rather large amount of autopsy data showed that low thyroid patients survived the usual childhood infectious diseases thanks to the invention of antibiotics, and years later develop heart disease. Barnes also found that thyroid treatment was protective in preventing heart attacks, based on his own clinical experience. Likewise for diabetes, Dr. Barnes found that adding thyroid medication was beneficial at preventing the onset of vascular disease in diabetics. Again, blood tests are usually normal. New research like the Hunt Study confirms that Broda Barnes was right all along, creating a paradigm shift in thyroid treatment, and constituting a frontal assault on the Institution of Medicine's thyroid dogma. (see image above)
 Above Image: Hunt Dog Courtesy of Wikimedia Commons.
Above Image: Hunt Dog Courtesy of Wikimedia Commons.The Hunt Study -
Thyroid Function and Mortality from Heart Disease
TSH is short for thyroid stimulating hormone, made by the pituitary gland. TSH actually stimulates the thyroid gland to make more thyroid hormone, and can therefore be used as a barometer of thyroid function. If thyroid function is low, the pituitary sends out more TSH to stimulate the thyroid to make more thyroid hormone.
Mainstream Medical Practice regards the TSH as the single most important test for determining thyroid function. High TSH means low thyroid function, and a Low TSH means normal or high thyroid function.
 What Did The Hunt Study Find?
What Did The Hunt Study Find?
 The Hunt Study from the April 2008 Archives of Internal Medicine examined mortality from coronary heart disease (CHD) and TSH level. The authors conclude, "The results indicate that relatively low but clinically normal thyroid function may increase the risk of fatal CHD."
The Hunt Study from the April 2008 Archives of Internal Medicine examined mortality from coronary heart disease (CHD) and TSH level. The authors conclude, "The results indicate that relatively low but clinically normal thyroid function may increase the risk of fatal CHD."
Right Image: Thyroid Gland makes thyroid hormone.
The Hunt Study measured thyroid function with the TSH test in 17,000 women and 8,000 men with no known thyroid disease or heart disease. All patients had "normal TSH" levels meaning the TSH values were in the lab reference range of 0.5 to 3.5. The women were stratified into three groups, lower TSH, intermediate and upper TSH levels, and mortality from heart disease was recorded over an 8 year observation period.
(see chart below).
70% Increase in Heart Disease Mortality for TSH in Upper Normal Range
 The Hunt study found that group with the higher TSH had a 70% increased mortality from heart disease compared to the lower TSH group. Remember all these TSH vales were in the normal lab range. See chart below for results of the Hunt Study:
The Hunt study found that group with the higher TSH had a 70% increased mortality from heart disease compared to the lower TSH group. Remember all these TSH vales were in the normal lab range. See chart below for results of the Hunt Study:
Left Image: Heart with Occluded Coronary Artery and Infarction at the apex, courtesy of wikimedia commons.
Results of the Hunt Study below:
| TSH | Death from Heart Disease | |
| Group 1 | 0.50-1.4 | baseline risk |
| Group 2 | 1.5-2.4 | 40% higher than baseline |
| Group 3 | 2.5-3.5 | 70% higher than baseline |
This Finding is Earthshaking !!
Thyroid Hormone Also Improves LDL Lipo-Proteins
Another report from the Hunt Study published in 2007 showed that LDL cholesterol was linearly associated with TSH level. (see chart below).
Note that TSH always remains within in the lab "normal range" (0.5-3.5).

Above chart shows linear increase in LDL cholesterol as TSH increases. Image Courtesy of Hunt Study European Journal of Endocrinology, Vol 156, Issue 2, 181-186, 2007
The Conclusion is Clear
The best way to normalize lipoprotein profile and reduce mortality from heart disease is to reduce TSH to the lower end of the normal range with thyroid medication. A TSH in the upper end of the normal range is associated with increased cardiovascular mortality and elevations in LDL lipo-protein measurements. A TSH at the lower end of the normal range is associated with protection from heart disease.
Statin Drugs or Thyroid to Prevent Heart Disease in Women?
 My previous article discussed the issue of statin drugs for women. Decades of published statin drug studies show that statin drugs simply don't work for women, and don't reduce mortality from heart disease in women. But on the other hand, the HUNT study shows that TSH levels in the lower normal range provide a 70% reduction in heart disease mortality for women. This can be accomplished safely with inexpensive thyroid medication under a physician's supervision. So for women concerned about preventing heart disease, this is good news, pointing out a natural alternative to statin drugs that works much better.
My previous article discussed the issue of statin drugs for women. Decades of published statin drug studies show that statin drugs simply don't work for women, and don't reduce mortality from heart disease in women. But on the other hand, the HUNT study shows that TSH levels in the lower normal range provide a 70% reduction in heart disease mortality for women. This can be accomplished safely with inexpensive thyroid medication under a physician's supervision. So for women concerned about preventing heart disease, this is good news, pointing out a natural alternative to statin drugs that works much better. Natural Thyroid is Better
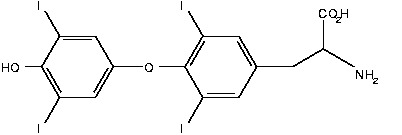
Above image: thyroid hormone Courtesy Wikimedia .
Rather than Synthroid, we prefer to use natural thyroid which is a dessicated porcine thyroid gland from RLC Labs or Armour Thyroid. The reason for this is that we have seen better clinical results with the natural thyroid preparations compared to synthroid.
Natural Thyroid is Safer, but can Cause Adverse Effects of Palpitations
Although natural thyroid is safe, there is always the possibility of adverse effects from thyroid excess, defined as too much thyroid medication. The first sign of thyroid excess is usually a rapid heart rate at rest or perhaps palpitations (at rest). We spend about five minutes at the office going over this adverse effect before starting patients on thyroid medication. Usually patients will notice the heart rate going up or the heart beat sounding louder than usual as the first sign that can be easily recognized. Once recognized, the patient is instructed to stop the thyroid medication, and symptoms usually resolve within 6 hours (for natural thyroid). It is perfectly safe to stop the thyroid medication at any time, as there will be no acute changes, merely a gradual reversion to the original state that existed before starting the thyroid pills.
Some patients are very sensitive to thyroid medication and will have thyroid excess symptoms such as rapid heart rate and palpitations from small amounts of thyroid medication. These are usually the elderly with underlying heart disease and/or magnesium deficiency, and we usually avoid giving thyroid medication to these patients. We also liberally supplement everyone with magnesium if their RBC magnesium levels are low.
About 5 per cent of our patients initially started on thyroid will notice symptoms of thyroid excess with a rapid heart rate, and they will stop the medication for a day or two and restart at a lower dosage with no problem. This is more common in Hashimoto's patients whose own production of thyroid hormones may fluctuate from month to month. Patients with magnesium deficiency or adrenal fatigue with low cortisol output on salivary testing will also tend to be more sensitive to small amounts of thyroid medication, so caution is advised in these groups as well.
Thyroid Excess Can Rarely Cause Atrial Fibrillation

Upper Image: EKG strip with Red Arrow shows atrial fibrillation, no recognizable P-wave.
Lower Image: EKG strip with normal rhythm with recognizable P wave (blue arrow). Courtesy of Wikimedia Commons.
So far, we have not had a patient go into atrial fibrillation from thyroid medication, probably because we spend so much time with each patient discussing the symptoms of thyroid excess, and the importance of stopping the thyroid medication if these symptoms are noted.
Mainstream Docs Don't Have Time To Discuss Adverse Effects
 One of the reasons the mainstream conventional docs will give only a minuscule amount of synthroid to the low thyroid patient is that they simply don't have the time to discuss thyroid excess and can't afford an adverse event which is more likely if the patient doesn't have a clue about what to watch out for. In addition, mainstream medical docs don't recognize the syndrome of adrenal fatigue or magnesium deficiency , so they can run into problems with thyroid excess without understanding why, and this also makes them very cautious, tending to under treat.
One of the reasons the mainstream conventional docs will give only a minuscule amount of synthroid to the low thyroid patient is that they simply don't have the time to discuss thyroid excess and can't afford an adverse event which is more likely if the patient doesn't have a clue about what to watch out for. In addition, mainstream medical docs don't recognize the syndrome of adrenal fatigue or magnesium deficiency , so they can run into problems with thyroid excess without understanding why, and this also makes them very cautious, tending to under treat.Left Image: Doctor thinking about thyroid dosage.
In patients with underlying heart disease who are prone to cardiac arrhythmias, thyroid excess can cause atrial fibrillation with characteristic EKG appearance. Atrial fibrillation can be a problem, because if it becomes chronic and doesn't go away on its own, the cardiologist will try a maneuver called cardioversion, the application of an electrical shock to restart a normal cardiac rhythm. Or, if that doesn't work, prescribe blood thinners, all of which is not without risk. So it is better to avoid atrial fibrillation altogether by simply stopping the thyroid pills whenever symptoms of rapid heart rate or palpitations are noted while at rest. Exercise induced rapid heart rate, of course, doesn't count since that is normal cardiovascular response to exercise.
How To Design A Better Hunt Study
How would I design an even better Hunt Study? That's easy. Include another group of patients with TSH levels above and below the study group, namely, below 0.5, and above 3.5. I would also include data on annual CAT coronary calcium scores. I would predict that the lower TSH group (below 0.5) would have even less heart disease than the higher TSH group, and that coronary calcium score, indicating plaque burden, would go up as TSH went up.
Articles on the Hunt Study from William Davis MD and Jacob Teitelbaum MD:
Hunt Study by William Davis MD
Hunt Study by Jacob Teitelbaum, MD.
Credit and Thanks is given to William Davis MD and Jacob Teitelbaum MD for bringing the Hunt Study to my attention.
For articles with related interest:
Saving Tim Russert and George Carlin
Reversing Heart Disease with Calcium SCore
Hypothyroid Type Two
Cholesterol Drugs for women
Jeffrey Dach MD
7450 Griffin Rd Suite 180/190
Davie, FL 33314
Phone: 954-792-4663
Blog
Links and References:
http://archinte.ama-assn.org/cgi/content/abstract/168/8/855
Arch Intern Med. 2008;168(8):855-860. Thyrotropin Levels and Risk of Fatal Coronary Heart Disease,
The HUNT Study
Arch Intern Med. 2008;168(8):855-860. Background Recent studies suggest that relatively low thyroid function within the clinical reference range is positively associated with risk factors for coronary heart disease (CHD), but the association with CHD mortality is not resolved.
Methods In a Norwegian population-based cohort study, we prospectively studied the association between thyrotropin levels and fatal CHD in 17 311 women and 8002 men without known thyroid or cardiovascular disease or diabetes mellitus at baseline.
Results During median follow-up of 8.3 years, 228 women and 182 men died of CHD. Of these, 192 women and 164 men had thyrotropin levels within the clinical reference range of 0.50 to 3.5 mIU/L. Overall, thyrotropin levels within the reference range were positively associated with CHD mortality (P for trend = .01); the trend was statistically significant in women (P for trend = .005) but not in men. Compared with women in the lower part of the reference range (thyrotropin level, 0.50-1.4 mIU/L), the hazard ratios for coronary death were 1.41 (95% confidence interval [CI], 1.02-1.96) and 1.69 (95% CI, 1.14-2.52) for women in the intermediate (thyrotropin level, 1.5-2.4 mIU/L) and higher (thyrotropin level, 2.5-3.5 mIU/L) categories, respectively.
Conclusions Thyrotropin levels within the reference range were positively and linearly associated with CHD mortality in women. The results indicate that relatively low but clinically normal thyroid function may increase the risk of fatal CHD.
Author Affiliations: Department of Public Health, Faculty of Medicine (Drs Åsvold and Vatten), and Human Movement Science Programme (Dr Nilsen), Norwegian University of Science and Technology, Trondheim, Norway; St Olavs Hospital, Trondheim University Hospital, Trondheim (Dr Åsvold); Department of Medical Biochemistry, Rikshospitalet-Radiumhospitalet Medical Center, Oslo, Norway (Dr Bjøro); and Department of Social Medicine, University of Bristol, Bristol, England (Dr Gunnell).
http://www.eje-online.org/cgi/content/full/156/2/181
European Journal of Endocrinology, Vol 156, Issue 2, 181-186, 2007
CLINICAL STUDY The association between TSH within the reference range and serum lipid concentrations in a population-based study. The HUNT Study
Bjørn O Åsvold1,2, Lars J Vatten1, Tom I L Nilsen1 and Trine Bjøro3
1 Department of Public Health, Faculty of Medicine, Norwegian University of Science and Technology, N-7489 Trondheim, Norway, 2 St Olavs Hospital, Trondheim University Hospital, Trondheim, Norway and 3 Department of Medical Biochemistry, Rikshospitalet-Radiumhospitalet Medical Center, Oslo, Norway (Correspondence should be addressed to L J Vatten
Jacob Teitelbaum MD
http://www.endfatigue.com/health_articles_f-n/Heart-low_thyroid_major_cause_heart_attacks.html
Jacob Teitelbaum, MD. Low Thyroid (Even if Tests are Normal) is a Major Cause of Heart Attacks,
William Davis MD
http://heartscanblog.blogspot.com/2008/06/is-normal-tsh-too-high.html
William Davis MD, begin quote:"Is normal TSH too high? There's no doubt that low thyroid function results in fatigue, weight gain, hair loss, along with rises in LDL cholesterol and other fractions of lipids. It can also result in increasing Lp(a), diabetes, and accelerated heart disease, even heart failure. But how do we distinguish "normal" thryoid function from "low" thyroid function? This has proven a surprisingly knotty question that has generated a great deal of controversy. Thyroid stimulating hormone, or TSH, is now the most commonly used index of the adequacy of thyroid gland function, having replaced a number of older measures. TSH is a pituitary gland hormone that goes up when the pituitary senses insufficient thyroid hormone, and a compensatory increase of thyroid hormone is triggered; if the pituitary senses adequate or excessive thyroid hormone, it is triggered to decrease release of TSH. Thus, TSH participates in a so-called "negative feedback loop:" If the thyroid is active, pituitary TSH is suppressed; if thyroid activity is low, pituitary TSH increases. An active source of debate over the past 10 years has been what a normal TSH level is. In clinical practice, a TSH in the range of 0.4-5.0 mIU/L is considered normal. (Lower TSH is hyperthyroidism, or overactive thyroid; high TSH is hypothyroidism, or underactive thyroid.) The data from a very fascinating and substantial observation called the HUNT Study, however, is likely to change these commonly-held thyroid "rules." endquote WIlliam Davis MD
International Hormone Society
http://www.intlhormonesociety.org/ref_cons/
Ref_cons_9_thryoid_treatment_of_clinically_hypothyroid_biochemically_hypothyroid_patients.pdf
International Hormone Society, references, clinically hypothyroid , lab euthyrroid
Other Blogs:
http://thyroid.blogspot.com/
Thyroid Blog by Dr. Richard B. Guttler M.D., F.A.C.E.
Location: Santa Monica, California, United States
http://www.stopthethyroidmadness.com/
Stop the Thyroid Madness Blog - a patient tries in vain to convince doctors to switch from Synthroid to Armour
Jeffrey Dach MD
7450 Griffin Road Suite 190
Davie, Florida 33314
954-792-4663
http://www.jeffreydachmd.com
http://www.drdach.com/
http://www.naturalmedicine101.com/
http://www.truemedmd.com/
http://www.bioidenticalhormones101.com/
For Disclaimer: Click Here
The reader is advised to discuss the comments on these pages with
his/her personal physicians and to only act upon the advice of his/her
personal physician. Also note that concerning an answer which appears as
an electronically posted question, I am NOT creating a physician —
patient relationship.
Although identities will remain confidential as much as possible, as I can not control the media, I can not take responsibility for any breaches of confidentiality that may occur.
Copyright (c) 2014 Jeffrey Dach MD All Rights Reserved
This article may be reproduced on the internet without permission,
provided there is a link to this page and proper credit is given.
FAIR USE NOTICE: This site contains copyrighted material the use of which has not always been specifically authorized by the copyright owner. We are making such material available in our efforts to advance understanding of issues of significance. We believe this constitutes a ‘fair use’ of any such copyrighted material as provided for in section 107 of the US Copyright Law. In accordance with Title 17 U.S.C. Section 107, the material on this site is distributed without profit to those who have expressed a prior interest in receiving the included information for research and educational purposes.
Serving Areas of: Hollywood, Aventura, Miami, Fort Lauderdale, Pembroke Pines, Miramar, Davie, Coral Springs, Cooper City, Sunshine Ranches, Hallandale, Surfside, Miami Beach, Sunny Isles, Normandy Isles, Coral Gables, Hialeah, Golden Beach ,Kendall,sunrise, coral springs, parkland,pompano, boca raton, palm beach, weston, dania beach, tamarac, oakland park, boynton beach, delray,lake worth,wellington,plantation
